May 11, 2023 — One of the deadliest cancers in cats, feline oral squamous cell carcinoma (FOSCC), moves quietly but quickly. Oral squamous cell carcinoma is not only the most common oral cancer in cats, but one of the most common feline cancers overall, accounting for roughly 8% to 10% of all cancers diagnosed. It's likely that many cat owners have encountered this dreadful disease if they've shared their lives with a feline friend.
Although FOSCC doesn't tend to spread beyond the head and neck, the cancer is still locally aggressive, burrowing deep into the bones of the jaw and oral cavity, making it nearly impossible to remove surgically. The tumors make eating and drinking difficult and are very painful. FOSCCs are resistant to chemotherapy but sensitive to radiation, and surgery often is combined with radiation to control the tumor. Unfortunately, side effects due to radiation are common, adding to a patient’s discomfort and impairing their quality of life. The average survival time is a dismal three months for cats diagnosed with this cancer.
New Treatments Desperately Needed
Since 2008, Morris Animal Foundation has stepped up research support for this terrible cancer. We've funded 18 studies with just over $1.5M invested in a wide range of projects focused on discovering new treatments to improve the quality of life for cats suffering from FOSCC.
From 2008 to roughly 2015, studies aimed to leverage advances in human-targeted cancer therapeutics in cats with FOSCC. Unfortunately, these approaches fell short when it came to efficacy in cats. However, one study showed promise.
Outsmarting FOSCC Tumors
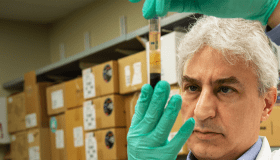
In a recently completed project, Dr. Erin Dickerson and her team at the University of Minnesota looked at blocking the process by which tumors mobilize nutrients for growth.
“Tumor cells are very greedy,” said Dr. Dickerson. “They’re selfish and hungry. They even convince other noncancerous cells around them to make food for them. This is called metabolic symbiosis. We set out to determine whether it existed in FOSCC and then see if we could exploit it.”
Dr. Dickerson’s secret weapon was an agent that disrupts lactic acid transport between tumor cells and fibroblasts, the noncancerous cells that tumor cells convince to supply them with food. The compound, which originally was developed to treat head and neck cancers in people, prevents the cancer cells from “eating” the lactic acid made by the fibroblasts. Dr. Dickerson’s team thought the same approach might work in cats, and the team was able to show that metabolic symbiosis was at play in FOSCC. They tested the new drug in cells in their laboratory with promising results. Unfortunately, the original agent is not available for cats, but a newer generation of similar compounds are in the development pipeline for people. Dr. Dickerson hopes that these, too will be effective in cats and ultimately commercially available.
Light Therapy and Nanotechnology
Other funded researchers are using light and a tumor cell targeted light-sensitive chemical to precisely trigger cancer cell death.
Utrecht University researcher Dr. Sabrina Santos Oliveira believes this approach would work in cats with FOSCC. Her team is studying a novel treatment called nanobody targeted photodynamic therapy.
Conventional photodynamic therapy uses light and a light-sensitive chemical to treat cancer. This chemical is given topically or intravenously to a patient, and then the light source is focused on any abnormal tissue. On their own, neither the light nor the chemical is harmful, but the light triggers the chemical agent to react with oxygen which in turn results in the production of harmful substances. These substances, known as reactive oxygen species, are toxic to the local cancer cells, ultimately leading to cell death.
Nanobody-targeted photodynamic therapy takes the process a step further, adding in tumor-cell targeted antibody fragments, coupled to the chemical, to target cancerous tissue more precisely. Light is used to trigger the chemical, but many of the pitfalls of conventional light-therapy are eliminated.
Dr. Michelle Oblak, from the University of Guelph, is also using nanotechnology in her new treatment study. Dr. Oblak is using nanoparticles known as porphysomes (pPs) that home in on tumor tissue. pPs can induce cell death when exposed to light (known as photodynamic therapy). This allows for precise killing of tumor cells without damage to nearby tissues. Dr. Oblak is conducting a pilot study to determine if this treatment will work in cats with FOSCC.
Other new studies include a study looking to find new therapeutic targets in progress at the University of Edinburgh, and a clinical trial at the University of Missouri which will use a new method of delivering radiation, known as lattice stereotactic body radiotherapy, to cats with FOSCC.
Together, these studies will hopefully inform the development of new treatment options to better care for cats with devastating oral cancer.
How You Can Help
Of course, studies like these take vision as well as financial investment. And that’s why Morris Animal Foundation, with the generous support of our donors, continues to fund this important work to change the odds for cats suffering from this devastating cancer.
Follow us to learn more about how our funded animal health research is helping cats live longer, healthier lives.